What causes ulcerative colitis?
No one knows for sure what causes ulcerative colitis or why it appears when it does. We do know that people who have family members with IBD are more likely to develop ulcerative colitis. One theory suggests that something, perhaps a virus or bacteria, affects the body’s immune system and triggers an inflammatory reaction in the intestinal wall. There is evidence that patients with this disease have abnormalities of the immune system. It is not known, however, whether the immune problems are a cause or a result of the disease.
Why is ulcerative colitis a concern?
Ulcerative colitis is a chronic illness that requires long-term medical care. The disease can be disabling when a patient is very ill. There may be remissions when symptoms go away for months or even years. However, symptoms usually return. For those patients whose colitis is significant, the lifetime risk of colon cancer is greater than normal, and it is important to see a doctor regularly so that they may monitor the patient’s overall health. Surgery to remove the colon may be necessary to cure the disease and minimize the risk of colon cancer. The CHOC IBD Program follows patients throughout their childhood and into early adulthood to help manage symptoms of ulcerative colitis and develop a treatment plan that adapts as the child grows and his or her needs change.
What are the symptoms of ulcerative colitis?
The following are the most common symptoms for Ulcerative colitis. However, each child may experience symptoms differently. Symptoms may include:
- Abdominal pain
- Bloody diarrhea
- Urgency to stool
- Fatigue
- Weight loss
- Loss of appetite
- Rectal bleeding
- Fever
- Growth failure.
The symptoms of ulcerative colitis may resemble other conditions or medical problems. It is important to consult a pediatric gastroenterologist for a proper diagnosis.
How is ulcerative colitis diagnosed?
Children and adolescents who have experienced chronic abdominal pain and bloody diarrhea may be examined for signs of Ulcerative colitis. In addition to a complete medical history and physical examination, diagnostic procedures for Ulcerative colitis may include:
- Blood tests. These tests help doctors look for anemia or chronic inflammation. They also show any changes in the child’s protein, vitamin and mineral levels. Sometimes blood tests can help distinguish between ulcerative colitis and Crohn’s disease. Learn more about blood tests.
- Stool tests. These tests look for evidence of blood loss or inflammation in the stool, or an infection by a parasite or bacteria causing the symptoms. Learn more about stool tests.
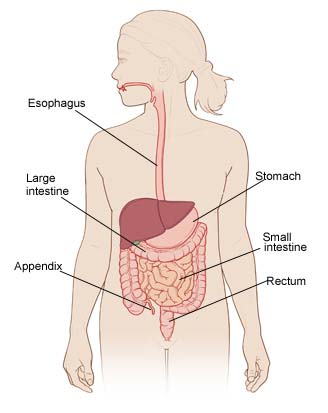
- Esophagogastroduodenoscopy (EGD or upper gastrointestinal endoscopy). A procedure in which a flexible scope is inserted through the mouth so that the child’s doctor can see abnormal growths, narrowing, inflamed tissues, ulcers and bleeding sites in the lining of the throat, esophagus, stomach and the beginning of the small intestine. During an endoscopy, doctors can also treat areas that are bleeding and take very tiny biopsies of tissues they would like to test. Learn more about upper gastrointestinal endoscopy. Learn more about endoscopy.
- Colonoscopy. A procedure in which a flexible scope inserted through the anus allows the doctor to see abnormal growths, narrowing, inflamed tissues, ulcers, polyps and bleeding sites in the view the large intestine and the final portion of the small intestine (distal terminal ileum). During a colonoscopy, the doctor can treat areas that are bleeding, remove polyps and take very tiny biopsies of tissues they would like to test. Learn more about colonoscopy.
- Push enteroscopy (push-pull enteroscopy or double balloon enteroscopy). A procedure that allows the doctor to see the small intestine that cannot be reached with traditional esophagogastroduodenoscopy. It is performed similar to an EGD. Biopsies can be taken during this study.
- Capsule endoscopy. A procedure that lets doctors see the parts of the small intestine that cannot be reached with traditional esophagogastroduodenoscopy. A video capsule is swallowed or placed in the intestine using an endoscope and passes through the intestine taking many pictures that can be compiled into a video. Biopsies cannot be taken during this study. Learn more about capsule endoscopy.
- Biopsy. Tiny, painless samples of tissue taken from the lining of the intestine for examination under a microscope in a laboratory. The samples are used to find abnormalities that cannot be seen with the naked eye and help determine more information about a patient’s disease. Taking a biopsy sample does not mean that the physician suspects a diagnosis of cancer.
- Upper gastrointestinal series (UGI,Upper GI, barium swallow). An X-ray that creates images of the organs of the upper part of the digestive system: the esophagus, stomach and duodenum (the first section of the small intestine). A fluid called barium (a chalky liquid) is swallowed and coats the inside of the intestine so that it will show up on the X-ray. This test is used to look at the anatomy and movement of the intestine. It is does not show abnormalities in the lining of the intestine as well as endoscopy. Sedation is not used for this test. Learn more about X-rays.
- Upper gastrointestinal series with small bowel follow through (UGI w SBFT). An X- test that creates images of the organs of the upper part of the digestive system including the entire small intestine (not just the first section). A fluid called barium (a chalky liquid) is swallowed and coats the inside of the intestine so that it will show up on the X-ray. This test is used to look at the anatomy and movement of the intestine. It is does not show abnormalities in the lining of the intestine as well as endoscopy. Sedation is not used for this test. Learn more about X-rays.
- Computed tomography enterography (CT of abdomen and pelvis, CTE). An X-ray of the intestine that gives a three dimensional view of the belly including the intestine and structures surrounding the intestine. This test uses oral and IV contrast and usually does not require sedation. Learn more about X-rays.
- Magnetic resonance enterography (MRI of abdomen and pelvis, MRE). An imaging test of the intestine that gives a three dimensional view of the belly including the intestine and structures surrounding the intestine. This test uses oral and IV contrast and may require sedation, depending upon the age of the patient. Learn more about MRI.
- Barium enema. An X-ray test that examines the organs of the lower part of the digestive system: the terminal ileum, colon and anus. Barium or another form of contrast is given through the anus as a controlled enema. This test is used to evaluate the anatomy and movement of the intestine. It may show strictures (narrowed areas) and obstructions (blockages) of the large intestine. It is does not show abnormalities in the lining of the intestine as well as colonoscopy. Sedation is not used for this test. Learn more about X-rays.
What is the treatment for ulcerative colitis?
At this time the only cure for ulcerative colitis is surgical removal of the large intestine. There are things that can be done to help control ulcerative colitis before surgery is desired or required. At CHOC, treatment plans are developed based on each patient’s unique medical, physical, social and emotional needs.
The goals of treatment may include:
- Correcting nutritional deficiencies
- Controlling inflammation
- Supporting optimal growth and weight gain
- Reducing symptoms so the child can live a more normal life.
Specific treatment will be determined by your child’s doctor based on the following:
- The child’s age, overall health and medical history
- The symptoms and extent of the child’s ulcerative colitis
- The child’s tolerance for specific medications, procedures or therapies
- The family’s opinion or preference.
Treatment may include the following:
Medication therapy. The child’s gastroenterologist may recommend one or a combination of medications that will help the intestine heal. The classes of medications available include aminosalicyclates, antibiotics, corticosteroids, immunomodulators and biologic therapies.
Diet and vitamin supplements. No specific food can be blamed as the cause of ulcerative colitis, although dietary changes may help control symptoms. Good nutrition is an important part of each patient’s overall treatment plan. Vitamin and mineral supplements—especially iron, zinc, calcium and vitamin D—can be very important to the healing process. Probiotics may be an important addition to help control symptoms.
Children with ulcerative colitis may lose weight because they are not getting enough calories because:
- They may avoid eating to prevent pain that comes with digestion.
- They have greater nutritional needs than average because of their disease.
- They may not be enthusiastic about eating when favorite foods are eliminated from their diet.
Some dietary changes may help control symptoms. In some cases symptoms are made worse by milk, alcohol, hot spices or fiber, but this may not be true for everyone. Huge doses of vitamins are ineffective in treatment and may even cause harmful side effects. Our gastroenterologist and dietitian can work with patients and families to determine possible foods to avoid and foods to emphasize.
The use of nutritional therapies as a sole treatment for Crohn’s disease is a controversial topic that needs discussion on a case-by-case basis. Nutritional supplements or special high-calorie liquid formulas may sometimes be suggested. It is rare, but possible, that a patient will need intravenous (by vein) feeding to support their nutrition during challenging stages of their treatment plan. Learn more about total parenteral nutrition (TPN).
Hospitalization. Children with ulcerative colitis are sometimes sick enough to need hospitalization to correct malnutrition and to stop diarrhea and the loss of blood, fluids and mineral salts. The patient may need a special diet, feeding through a vein, medications, and, in some cases, surgery.
Surgery. Most children with ulcerative colitis do not need surgery. However, about 25 to 40 percent of children with ulcerative colitis eventually require surgery for removal of the colon because of massive bleeding, chronic debilitating illness, perforation of the colon, or risk of cancer. Sometimes, removing the colon is suggested when medical treatment fails or the side effects of medications threaten the patient’s health. Learn more about surgery at CHOC.
The common surgical options:
- Proctocolectomy with ileostomy. The most common surgery is the proctocolectomy (removal of the entire colon and rectum) with ileostomy (creation of a small opening in the abdominal wall where the tip of the lower small intestine, the ileum, is brought to the skin’s surface to allow drainage of waste).
- Ileoanal reservoir surgery (J-pouch among other terms). This is an alternative to a permanent ileostomy and uses part of the small intestine to create a pouch near the rectum to hold stool for evacuation at a later time. The muscle of the rectum is left in place, so the stool in the pouch does not leak out of the anus. People who have this surgery are able to control their bowel movements. Learn more about surgery at CHOC.
What is the long-term outlook for a child with Ulcerative colitis?
Ulcerative colitis is a chronic condition that may recur or flare at various times over a lifetime. Children may experience physical, emotional, social and family problems as a result of the disease, increasing the importance of proper management and treatment of the condition at a comprehensive, long-term program like the IBD Program at CHOC.
The following chart summarizes some of the problems children may face.
| Emotional Responses | Social Problems | Effects on the Family |
|
|
|
At CHOC our multidisciplinary team includes a dedicated dietitian, social worker and case manager who work with families and patients to make life with ulcerative colitis more manageable. Our psychology department is readily available to help patients deal with chronic illness and develop the skills it takes to cope on their own in daily life. Our team provides ease of access to all our resources including office visits, group teaching sessions and educational materials.